The correlation between radiation exposure and increased cancer risk is based not on clinical studies of medical imaging patients, as most reporting would suggest, or as a reasonable person might conclude.
The correlation is based on speculation, using the only quantitative data available, which primarily consists of a 70 year-long study of Hiroshima and Nagasaki survivors, along with more recent studies of patients who received massive amounts of radiation as part of their treatment for Leukemia and other cancers.
Cancers of the breast, bladder, colon, liver, lung, esophagus, ovaries, stomach and more have been linked with simultaneous, high-dose exposure, greater than 50,000 mrem or 500 mSv. Clearly, the cancer risk is there when an individual is exposed to massive amounts of ionizing radiation.
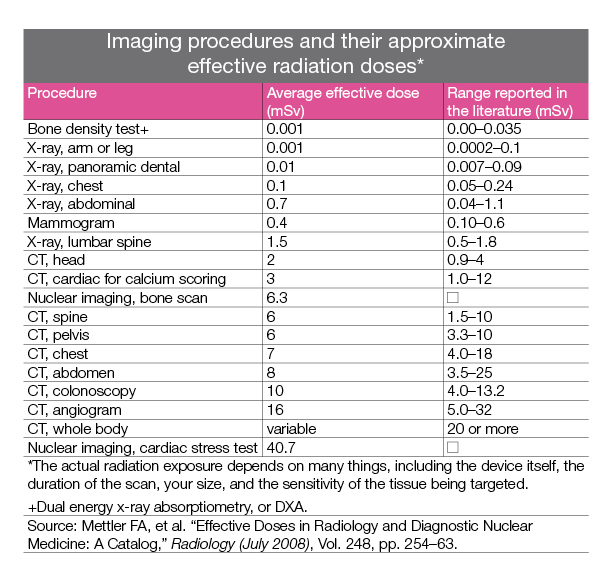
But we’re not talking about exposure to 500 mSv in a single dose. No medical imaging test does that. We’re talking about the .4 mSv exposure of a mammogram.
Does an annual mammogram (0.3 to 0.44 mSv) present a true cancer risk when it is acceptable for a pilot or flight attendant to be exposed to an additional 20 mSv per year? In other words, wouldn’t it take the average woman more 50 years of annual mammograms before her dose equals that which a pilot is allowed in one year? And more than 1,200 years of annual mammograms before she is exposed to the 500 mSv equivalent of a Hiroshima survivor?
Furthermore, is there any data to suggest that the cumulative effect of many years of modest radiation exposure equals the effect of an atomic bomb blast where the massive radiation dose was delivered all at once and to all organs of the body simultaneously?
The American Association of Physicists in Medicine, an organization of more than 7000 medical physicists responsible for the quality and safety of medical imaging and radiation therapy, approved in December 13, 2011 the following statement concerning the risks of medical imaging (3):
The American Association of Physicists in Medicine (AAPM) acknowledges that medical imaging procedures should be appropriate and conducted at the lowest radiation dose consistent with acquisition of the desired information. Discussion of risks related to radiation dose from medical imaging procedures should be accompanied by acknowledgment of the benefits of the procedures. Risks of medical imaging at patient doses below 50 mSv for single procedures or 100 mSv for multiple procedures over short time periods are too low to be detectable and may be nonexistent.
Predictions of hypothetical cancer incidence and deaths in patient populations exposed to such low doses are highly speculative and should be discouraged. These predictions are harmful because they lead to sensationalistic articles in the public media that cause some patients and parents to refuse medical imaging procedures, placing them at substantial risk by not receiving the clinical benefits of the prescribed procedures.
Highly speculative articles that predict cancer incidence and death in populations receiving relatively small doses of radiation from medical imaging are not without their own health risks. These articles receive considerable media attention because they emphasize hypothetical cancer risks of imaging procedures without acknowledgment of the benefits that the procedures provide to patients. Governmental agencies, institutions, and medical groups spend millions of dollars each year to safeguard against low levels of radiation—funding that is diverted from other more pressing needs. This distorted emphasis does induce one risk in many patients—namely anxiety about imaging procedures that causes some patients and parents to delay or defer necessary imaging procedures. The negative health consequences of deferred imaging examinations undoubtedly far outweigh any risks of having the procedures performed.
-
- Estimates of cancers and cancer deaths resulting from medical imaging procedures that use ionizing radiation are computed by multiplying very small hypothetical risks by large patient populations to yield thousands of “cancer victims.”
- The hypothetical, highly speculative risks are obtained from tabulations in the Biological Effects of Ionizing Radiation VII report based primarily on data from survivors of the Hiroshima and Nagasaki atomic explosions, a population greatly different from patients experiencing medical imaging.
- To estimate the risks at low doses delivered by medical imaging from data greater than 100 mSv acquired from the Japanese studies, the linear no-threshold model of radiation injury is used, even though considerable evidence suggests that it is an inappropriate model for risk estimation.
- Publications that estimate cancers and cancer deaths caused by medical imaging are frequently sensationalized by electronic and print public media, resulting in considerable public anxiety and fear about medical imaging.
- On some occasions, the fear and anxiety results in reluctance to accept imaging procedures, even though the risk of a deferred examination creates a much greater risk than that related to radiation from the procedures, if any risk exists at all.
Physicians often say, “We just don’t know what the long-term, cumulative effects of radiation are.” Maybe so. But we do know what the benefits of mammographic screening are, in terms of early detection and lives saved.
And as for the cumulative nature of radiation, consider this: Many flight crews begin their career—along with the associated higher radiation exposure—during their early 20s. Shouldn’t we now be seeing the cumulative effects of radiation exposure in these individuals after they retire? Do pilots and flight attendants die at a younger age than the average American? While rumors abound, there is no clinical study to date that has shown a lower life expectancy for flight crews. In fact, one study demonstrated that retired pilots actually have greater longevity than the population as a whole.
Perhaps the phrase “once and for all” in the title of this section is wishful thinking. You can bet your bottom dollar that there will be a story on the “dangers” of radiation in medical imaging on the news within the next couple of months.
But at least now, you’ll know the truth.